Serious Downturn In Children’s Health Coverage Rates In California After Years Of Improvement, Covid-19 Threatens Worsening Outcomes

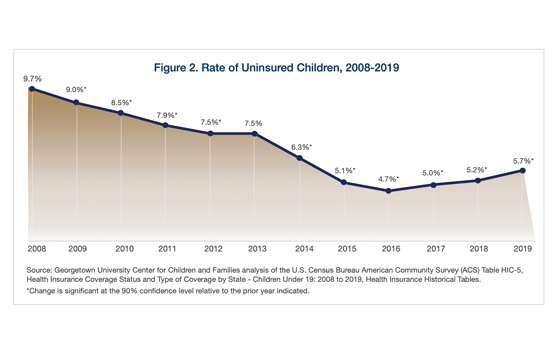
Children’s health coverage is critical in ensuring kids are on the path to succeed in school and in life. We know that when children have access to comprehensive quality care, they are healthier and more likely to enter school ready to learn and reach graduation. Overall, California has made huge strides in recent decades to ensure more families and children are healthy and excel in life, particularly by increasing access to health coverage. In fact, we reduced the number of uninsured children from 2 million in 1999 to just over 300,000 in 2016. However, despite steady coverage gains up to 2016, recently published data by the Center for Children & Families of the Georgetown University Health Policy Institute show that too many children are losing ground on this critical factor and therefore cannot access regular and preventative health care in California and across the U.S.
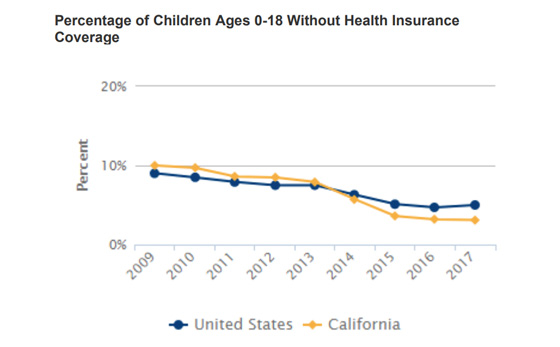
California has historically had a significant number of uninsured children when compared to other states. In fact, in 2009, 10% of the state’s children – over 1,100,000 kids – were uninsured, even though children made up 30% of the total population. With the introduction of the Affordable Care Act (ACA), which went into effect in 2014, and subsequent decisions by California to extend eligibility for Medi-Cal to undocumented children, the number of uninsured children would go on to decrease from 7% (over 700,000) to 3% (over 300,000) between 2013 and 2015.
Nationwide, the number of uninsured children increased by about 320,000 in 2019 alone, jumping back up to a 5.7 percent uninsured rate. This is the biggest one-year loss of children’s coverage and the first significant increase of uninsured children in a decade, according to the new report. An estimated 4.4 million children were uninsured nationwide in 2019, with a total increase of 726,000 uninsured children since 2016. This alarming report also found that much of the health coverage gains for children following implementation of the ACA have now been eliminated.
Where all California children are eligible for health insurance, it is estimated that 334,000 – or about 3.6% – of children remain without health coverage in 2019. The report indicates that five California counties – Los Angeles, San Diego, Orange, San Bernardino, and Riverside – were among the top 20 counties in the U.S. with the highest number of uninsured children, placing CA’s state ranking at 49 out of 51, inclusive of Washington D.C. (it’s important to note that this ranking is of the total actual number of uninsured children, not per capita). Further, the uninsured rate for Latino children was 4.4% in 2019 – 1.5 times higher than white, non-Latino children in California. Since the increase in the number and rate of uninsured children occurred prior to the pandemic, the situation is likely much worse for CA children and families in 2020.
This troubling data shines an unflinching light on concerns advocates and families alike raised nearly two years ago; families are being discouraged from enrolling in benefits available to them out of fear because of anti-immigrant policies and sentiment as well as virulent nativist rhetoric. Since the Trump Administration took charge in January 2017, the uninsured rate for children increased every year, from the historic low of 4.7% in 2016 to 5.7% in 2019. This is no coincidence; in fact, in addition to its aggressive anti-immigrant policies and pronouncements, this administration made it abundantly clear that it would do everything possible to repeal the ACA. Efforts to repeal the ACA failed in Congress, but now a Texas federal court case seeking to overturn the ACA is before the U.S. Supreme Court. It is hard to avoid the conclusion that years of hostility to both the ACA and to immigrants has served to sabotage the ACA’s effectiveness in expanding coverage for children, among other ways.
Below are just a few ways that the Administration has constricted the ACA and thus reduced enrollment rates:
- Reducing Outreach: In August of 2017, the U.S. Centers for Medicare and Medicaid Services announced a 90% cut to the advertising budget.
- Cutting Marketplace Subsidies: Approximately 7.3 million marketplace enrollees would see their premiums increase.
- Promoting Counterproductive Waivers: Such waivers imposed work requirements and administrative burdens on adults benefitting from the ACA’s Medicaid expansion.
Perhaps most impactful for California – with the largest immigrant population in the nation – was the September 2018 proposal and subsequent decision to change the public charge rule allowing immigrants’ applications for permanent residency to be denied due to being eligible for a broader range of safety-net programs. This chilling effect is not limited to immigrant only households; in fact, it also impacts mixed-status households where children may be citizens but one of their parents may not be. California has done everything in its power to ensure these populations were covered, all at the state’s sole cost.
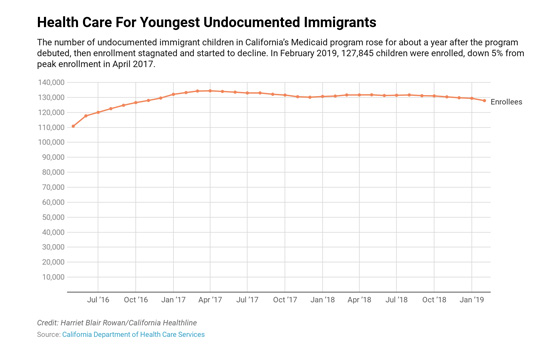
California expanded Medi-Cal eligibility to children under 19 years of age regardless of immigration status, with the passage of SB 75 in May of 2016. This led to a peak enrollment of 134,000 of undocumented children in April 2017; however, these numbers would plateau and eventually begin to decline due to rising concerns about attitudes toward immigrant populations, namely through the public charge rule and general hostility from the federal administration.
Perhaps the most worrying takeaway from this data is the fact that it doesn’t even take into account how the COVID-19 pandemic will further exacerbate declining enrollment numbers. As a record number of people are unemployed, employer-based health coverage rates will decline, which will see an increase in the need for Medicaid coverage.
Ultimately, California might not have the financial means to increase Medi-Cal outreach or expand coverage in the midst of an unprecedented economic downturn, especially with the lack of further federal stimulus. Congress must step up if it wishes to more effectively combat the spread of COVID-19. If people do not have access to some form of health insurance, they will forgo seeking out treatment in fear of the financial consequences. This will be counterproductive in our efforts as a nation to deter the spread of COVID-19. Congress can help states immediately in one of two ways:
- Issuing a Deportation and Detention Moratorium: Not only is the spread of COVID-19 in Immigration and Customs Enforcement detention and transfer centers more deadly than anywhere else, but it is also causing fear in people to seek out and receive medical treatment that is vital in fighting COVID-19.
- Pass the HEROES Act: The HEROES Act includes a number of provisions that would enhance Medicaid funding, provide COBRA subsidies for employees, and would require a broad special enrollment period.
It is unfathomable that during a global pandemic families and children are facing the potential elimination of the ACA. Millions of families face being kicked off their. If Congress does not step up and take decisive action, decades of progress will have been lost and generations of children will grow up without the comprehensive health care we know makes the difference for them to lead healthier, happier lives.
California has a history of leading the nation in a number of “firsts.” It is for this reason that we cannot wait idly as thousands of children are unenrolled. Although California might struggle to find the financial means to reach previous rates as long as the COVID-19 induced recession continues, we can look to the philanthropic sector to prioritize efforts to find and enroll all eligible children in health coverage. Additionally, the Legislature should continue its efforts to explore options for increasing enrollment rates in public programs through horizontal integration and express lane eligibility processes. United Ways of California will continue to support health coverage for all people both through robust advocacy efforts at the state and federal level and with the work of local United Ways in conducting outreach and enrollment into health coverage for Californians.